The RULA method
The RULA (Rapid Upper Limb Assessment) method was developed to assess the postural and biomechanical stresses exerted on the upper limbs of workers.

The RULA (Rapid Upper Limb Assessment) method mainly assesses the upper limbs (shoulders, elbows, wrists), but also the neck and trunk. It applies to tasks in which the operator mainly uses his or her upper limbs, with or without movement. Postures are mainly studied by taking into consideration adjustments relating to the force applied and the repetitiveness of the gesture.
This method complies with European Directive 90/270/EEC. It highlights the postural risk associated with the work cycle observed, and produces a postural risk score.
Validated by several studies, the RULA method is used by many health and safety professionals around the world.
This method is not recommended for assessing manual handling tasks.
The RULA method primarily assesses posture, but takes into account parameters related to force, repetitiveness or muscular activity. However, it focuses mainly on the analysis of working postures.
It does not take into account activity duration, recovery time or vibration.
A separate assessment of the left and right sides is essential when using RULA. There is no method for combining the two scores to obtain an overall result for the whole body.
The cumulative effects of all the activities involved in a job or task are not taken into account.
Analysis of the request and development of criteria for selecting the work situations to be observed.
Assessment of critical postures using RULA-type postural assessment methods to estimate postural risk levels.
Analysis of postural data to draw up a list of priorities and seek solutions and proposals for improvement.
Formulation of improvements based on the results of the analysis, and implementation of corrective measures taking into account the risks identified.
A new assessment of the workstation enables us to study the impact of corrective measures on postural risk.
The RULA (Rapid Upper Limb Assessment) method involves an assessment in two main steps: analysis of the upper limbs, followed by assessment of the neck and trunk.
The steps to follow for this assessment are as follows:
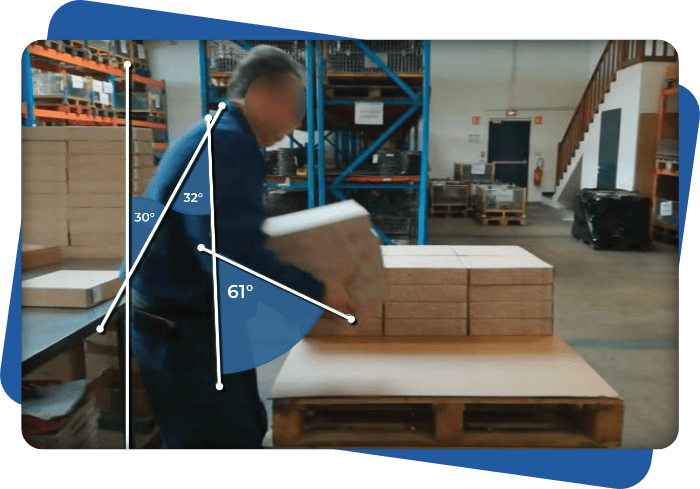
Using the illustration below, we apply the RULA method, following each step of the process in detail.
The aim is to calculate the RULA score corresponding to this assessment, and to identify the level of postural risk associated with the work activity analyzed.
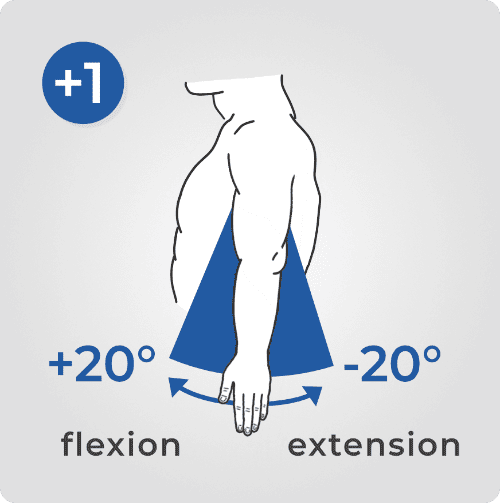
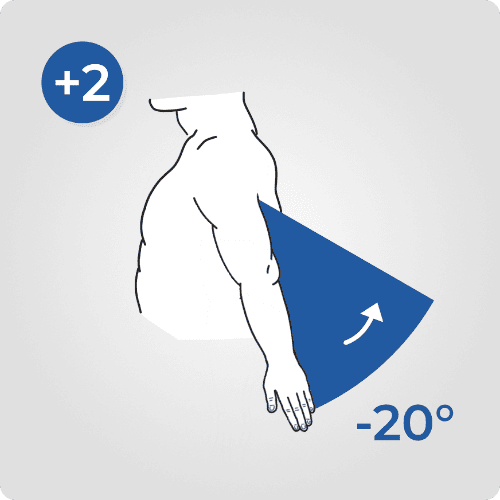
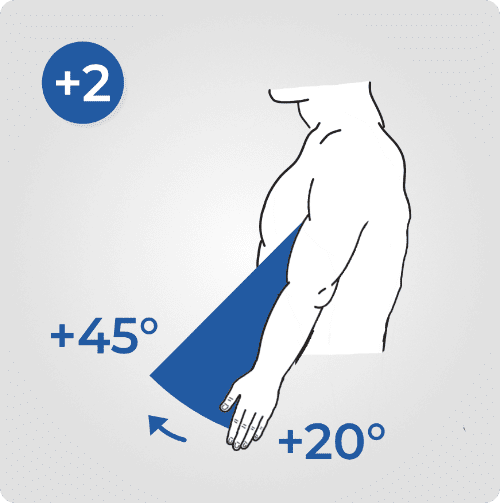
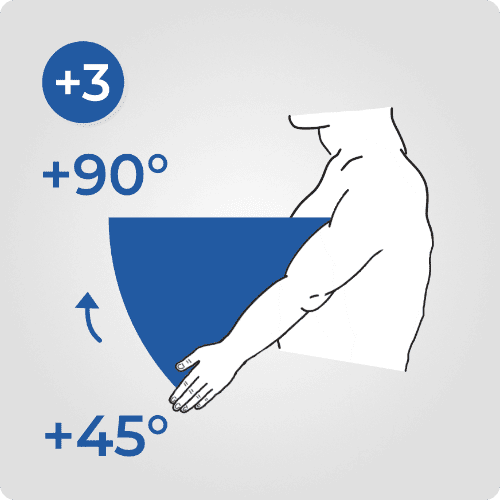
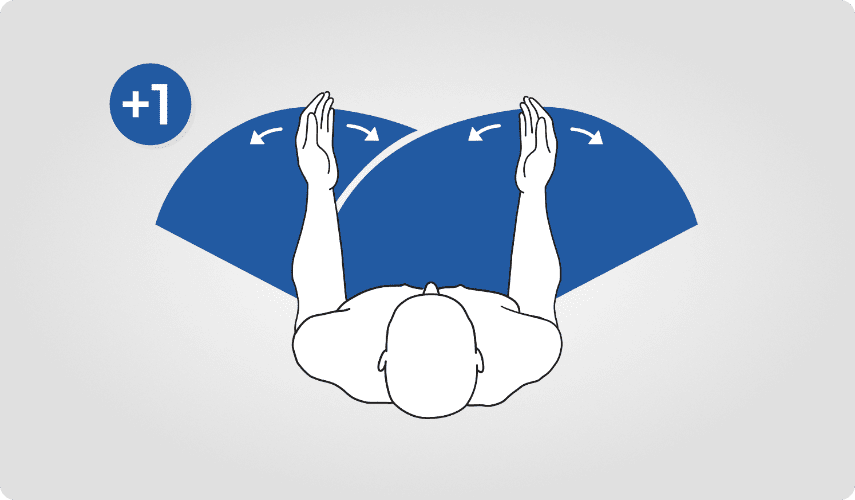
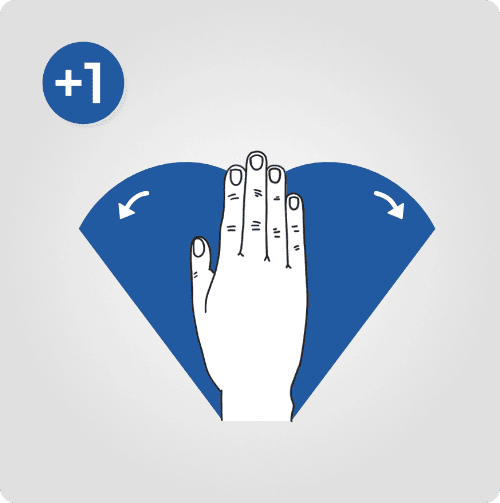
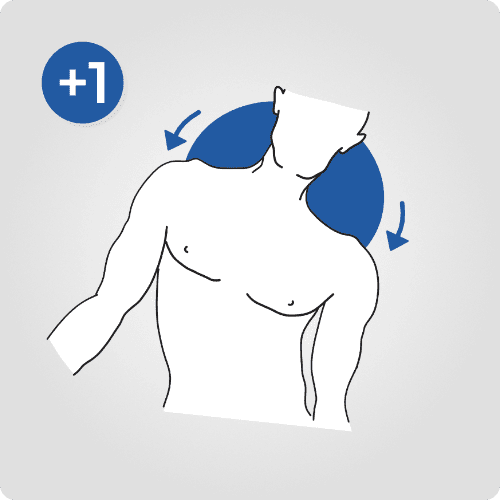
The shoulder score is between 1 and 6. It is based on the angle of flexion or extension of the shoulder and the abduction or support of the arm.
In our example, the shoulder is flexed 32° (i.e. between 20° and 45°): the score is (+2).
Adjustments :
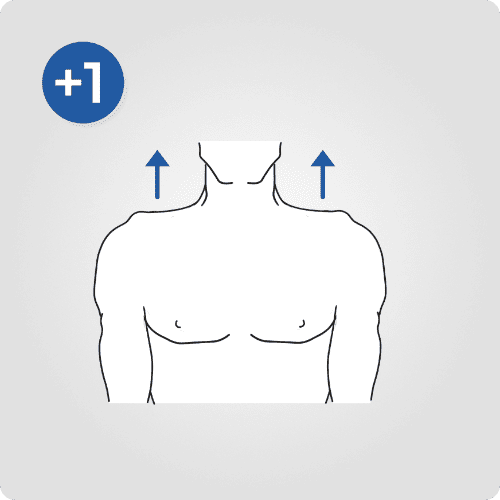
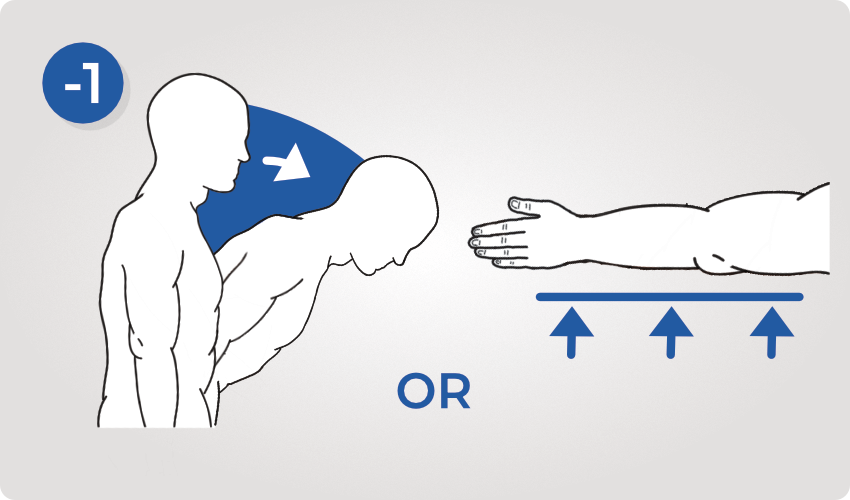
To the previous score, add +1 if the shoulder is raised, +1 if the arm is abducted and subtract -1 if the arm is supported or the person is bent over.
In our example: no adjustments.
Shoulder score :

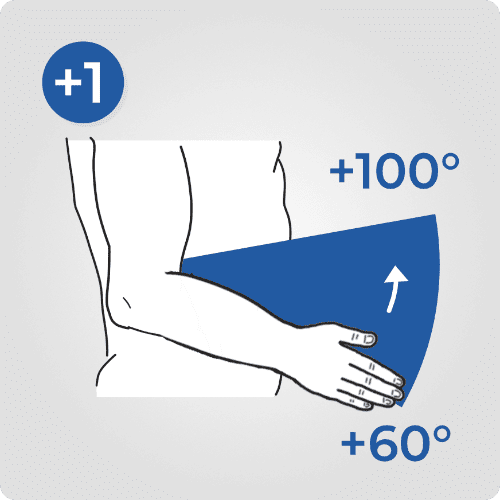
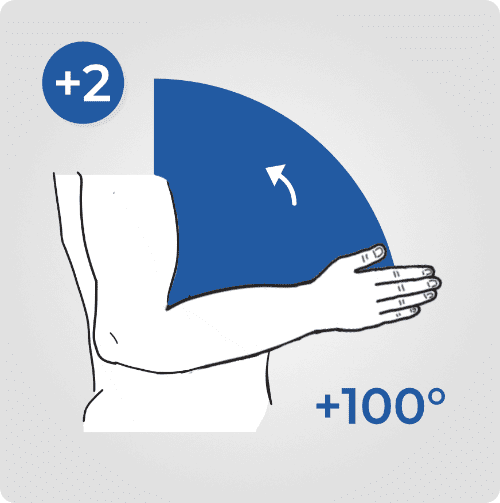
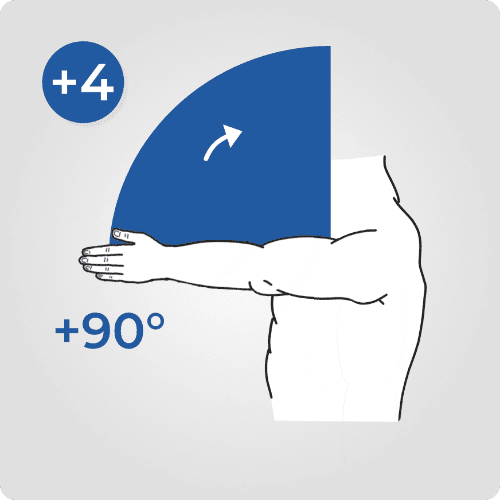
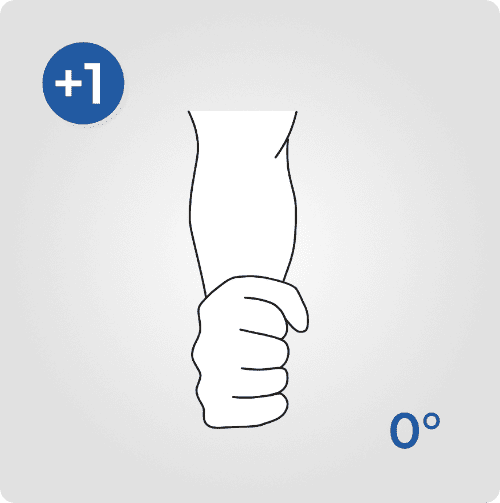
The elbow score is between 1 and 3. It is based on the angle of flexion of the elbow.
In our example, the elbow is flexed 61° (i.e. between 60° and 100°): the score is (+1).
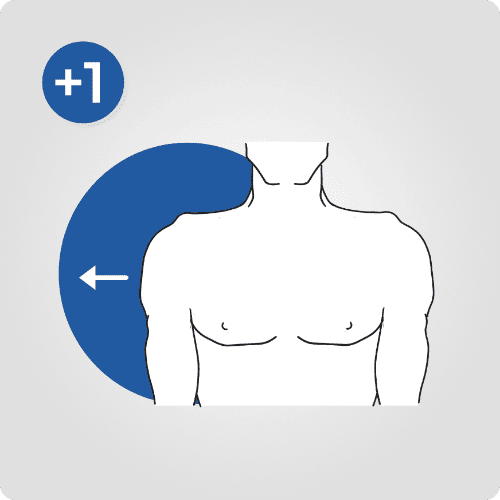
Adjustments :
Add +1 to the previous score if one of the arm movements is across the median line or outside the body.
In our example, the forearm remains in line with the body: no adjustment.
Elbow score :

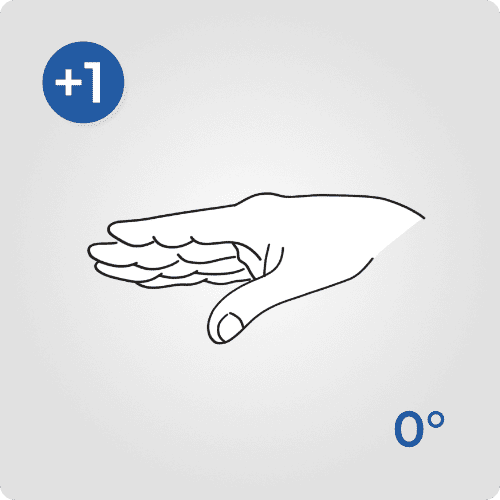
The wrist score ranges from 1 to 4. The score is based on the angle of flexion or extension of the wrist.
In our example, the wrist is not flexed: the score is (+1).
Adjustments :
Add +1 to the previous score if an ulnar/radial deviation of the wrist is observed.
In our example: no adjustments.
Wrist score :

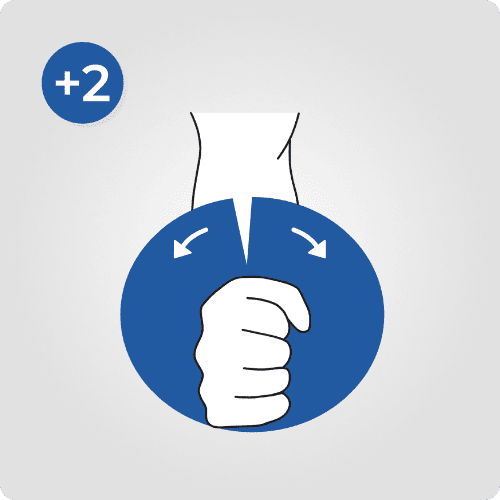
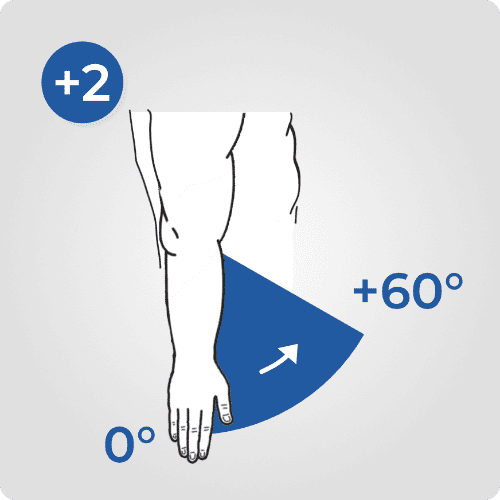
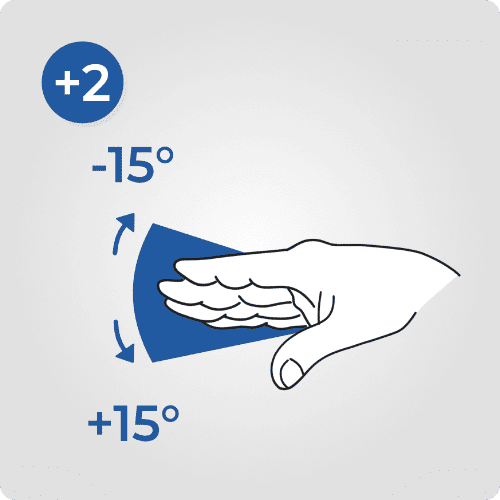
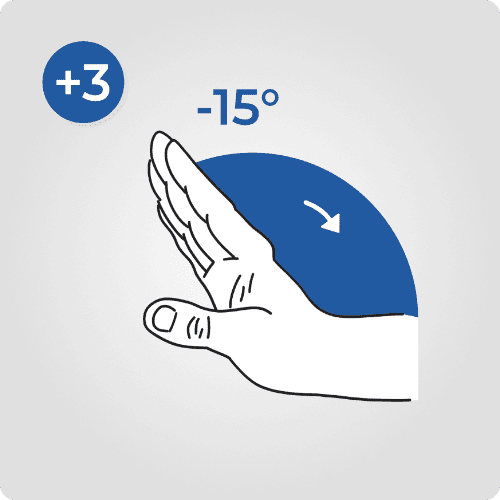
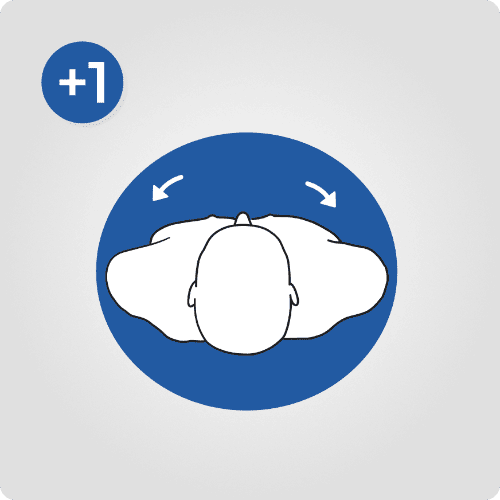
The forearm score is between 1 and 2. The angle corresponding to the rotational movement of the frontal and sagittal planes is described in the transverse plane.
The angle of pronation of the forearm corresponds to rotation in the direct direction, while supination corresponds to rotation in the indirect direction.
The amplitude is limited to 80° for pronation and 85° for supination.
In our example, pronation is observed: the score is (+1).
Wrist pronosupination score :


We will now cross-tabulate the scores obtained in steps 1 to 4 to obtain the result corresponding to group A, which includes the shoulder, elbow, wrist and pronation/supination of the wrist.
Group A score :

If the posture is held statically for more than 10 minutes or if the action is repeated more than 4 times per minute, add (+1). If these conditions are not met, no points need to be added.
In our example, no points need to be added (+0).
In our example, the person is carrying a load of between 2kg and 10kg intermittently, so we add (+1).
Add the values from steps 5 to 7 to obtain the score for group A, including the shoulder, elbow, pronation/supination of the forearm and wrist.
Adjusted score for group A :

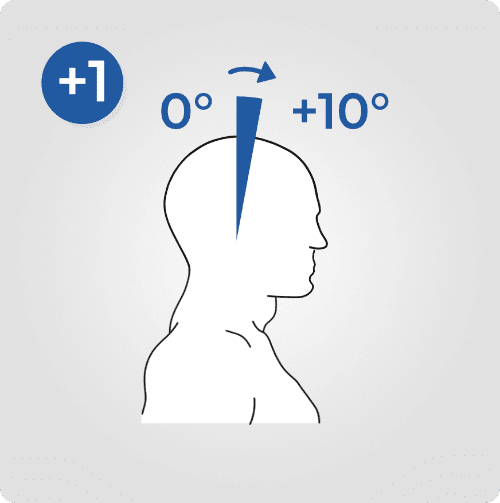
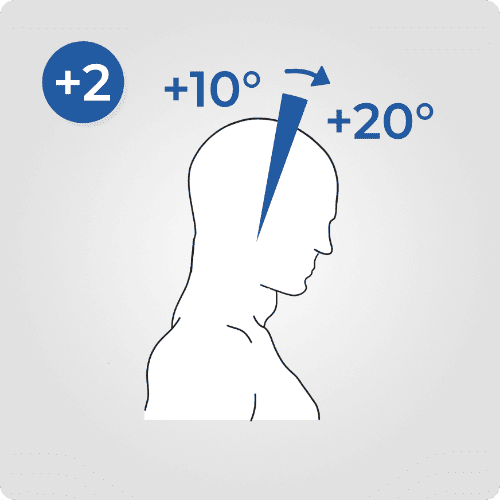
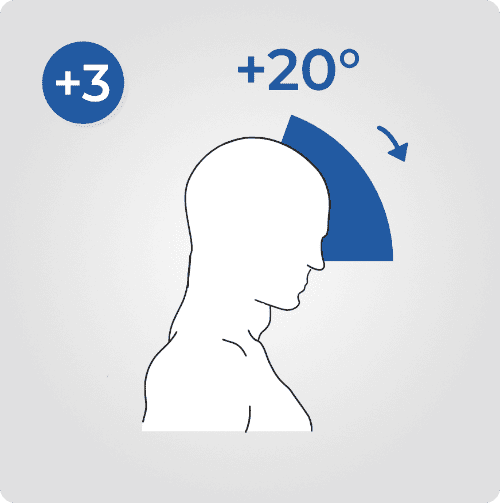
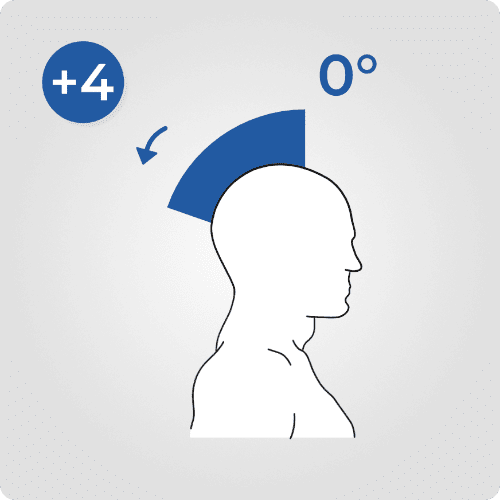
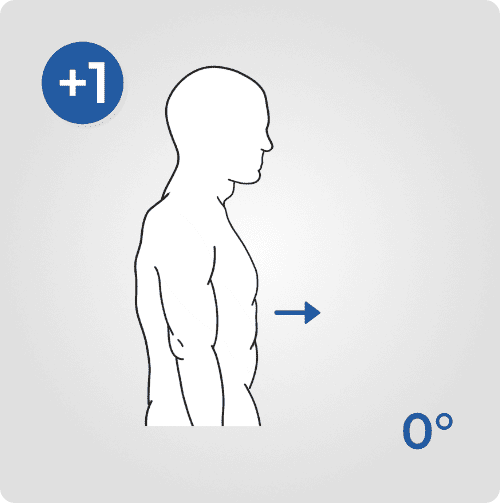
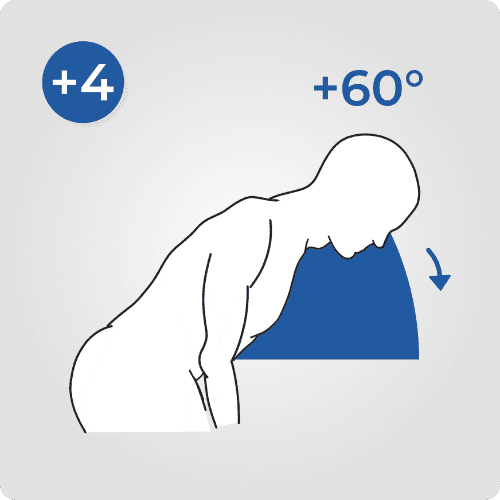
The neck position score is between 1 and 6. The score is based on the angle of flexion or extension of the neck, as well as any adjustment for axial rotation or lateral flexion of the neck.
Neck flexion is the forward movement of the head from a point of neutral neck position. Neck extension is the backward movement of the head from a point of neutral neck position. The neutral position corresponds to the position where the upper body is straight and you can see a visual target in front of you at eye level.
In our example, the neck position is between 0 and 10°: the score is (+1).
Adjustments :
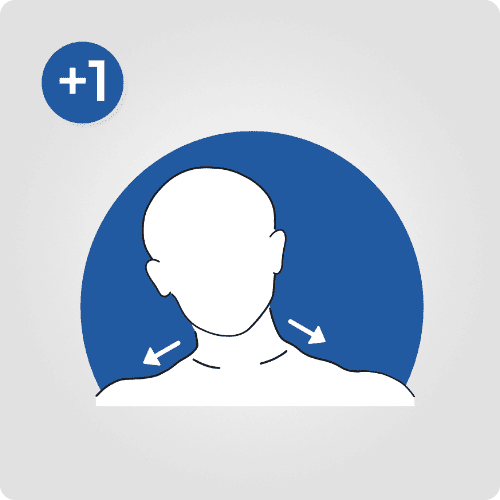
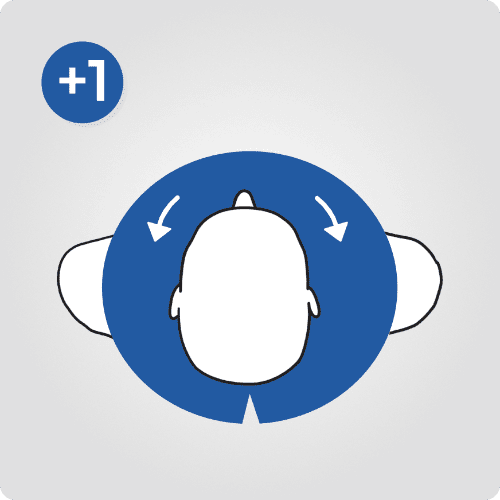
Add +1 to the previous score if there is lateral flexion or rotation of the neck.
In our example: no adjustments.
Neck score :

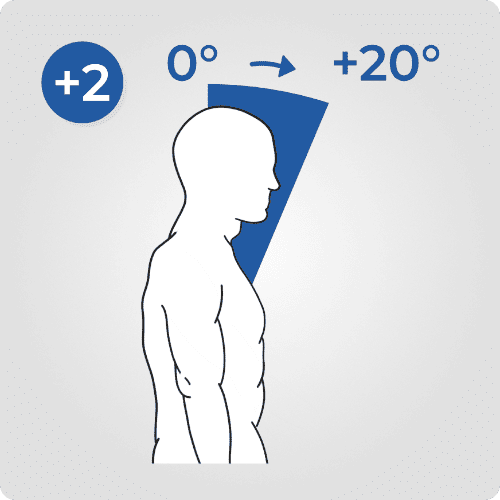
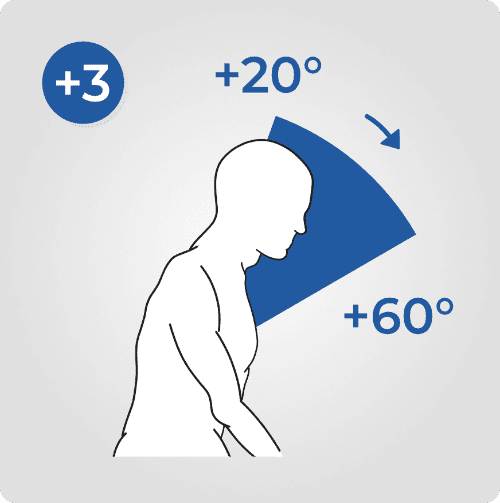
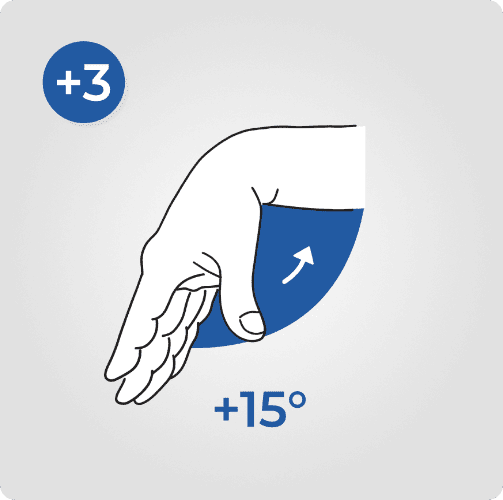
The trunk position score is between 1 and 6. It is based on the angle of flexion of the trunk, as well as axial rotation or lateral flexion of the trunk.
Trunk flexion corresponds to the rotation of the frontal and transverse planes described in the sagittal plane.
In our example, the trunk position is 30° (i.e. between 20° and 60°) : the score is (+3).
Adjustments :
Add +1 to the previous score if there is lateral flexion or rotation of the trunk.
In our example: no adjustments.
Trunk score :

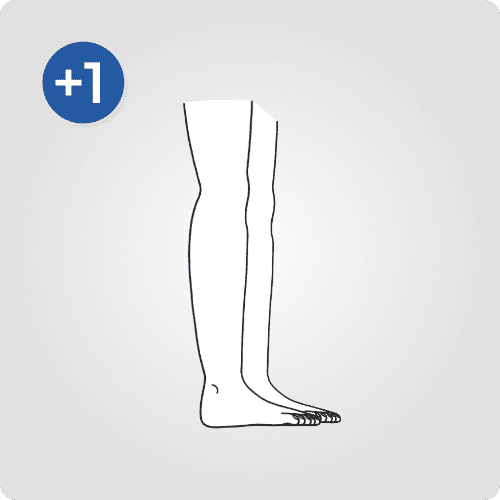
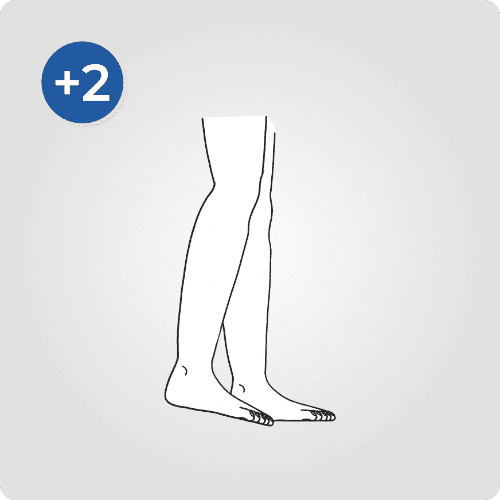
The leg position score is between 1 and 2. If the legs and feet are bipodal, the score is (+1). If the legs and feet are in monopodal support, the score is (+2).
In our example, the legs and feet are in bipodal support: the score is (+1).
Score legs :

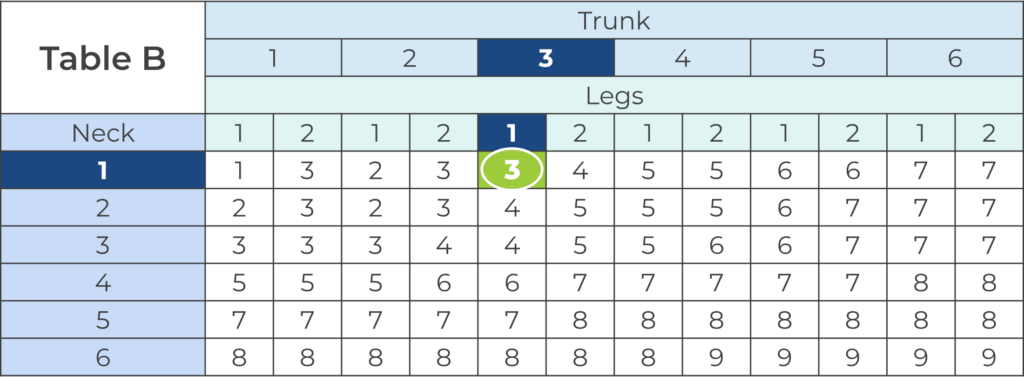
We will now cross-tabulate the scores obtained in steps 9 to 11 to obtain the result corresponding to group B, including the neck, trunk and legs.
Group B score :

If the posture is held statically for more than 10 minutes or if the action is repeated more than 4 times per minute, add (+1). If these conditions are not met, no points need to be added.
In our example, no points need to be added (+0).
In our example, the person is carrying a load of between 2kg and 10kg intermittently, so we add (+1).
Add the values from steps 9 to 11 to obtain the score for group B, including the neck, trunk and legs.
Adjusted score for group B :

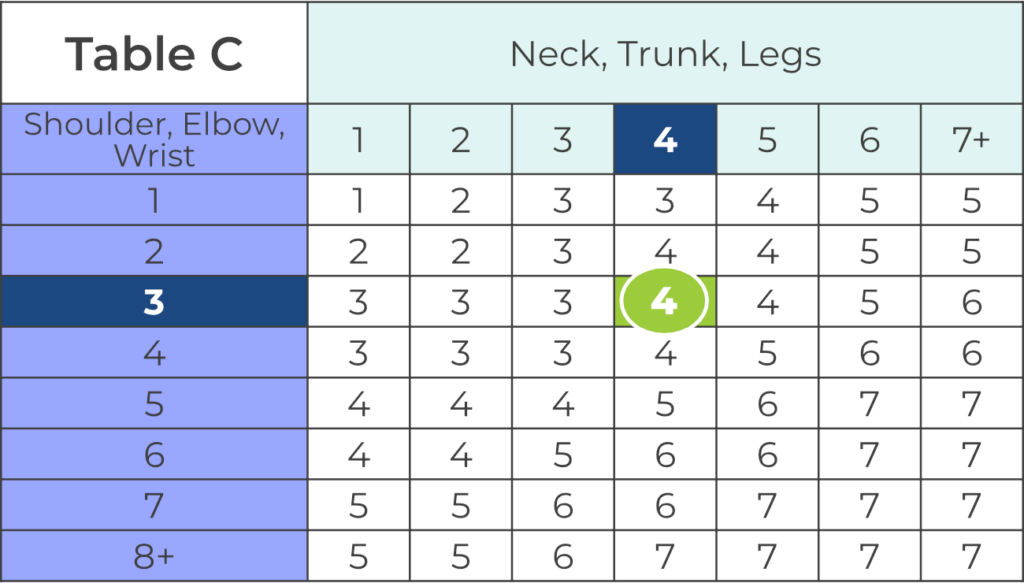
Finally, we cross-tabulate the values obtained from adjusted group A with the values from adjusted group B to obtain the score representative of postural risk, using table C.
RULA final score :

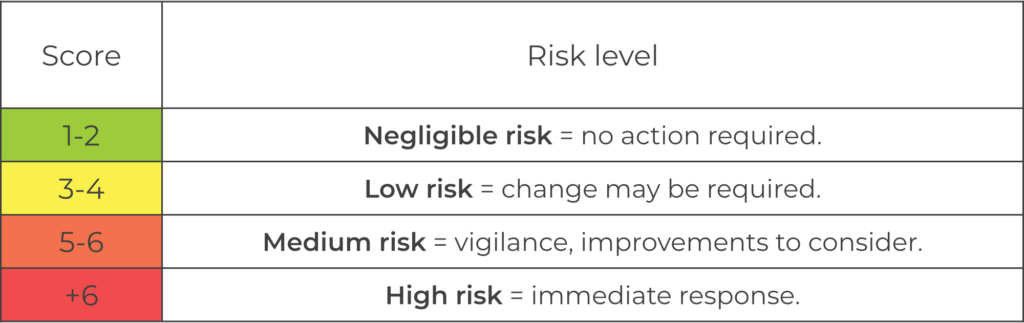
The RULA score represents the postural risk level of the work task being assessed. The minimum score is 1, and the maximum score is 7.
Table C shows the total score for A and B. Let’s assess the MSD risk according to the final score.
In our example, the final score of 4 indicates a low risk. A change may be necessary to improve work methods and thus reduce the risk of MSDs.
Nawo Live is your physical activity risk assessment tool for identifying risk factors for musculoskeletal disorders (MSDs).
In Nawo Live, automate and evaluate all biomechanical risk factors using reference methods (RULA, REBA, NIOSH, etc.).
Nawo Live guarantees you a reliability of the measurements acquired by our systems, including :
Newsletter